The Dutch Lung Cancer Audit: Nationwide Quality of Care Evaluation Using Quality Indicators
The final session was co-chaired by Matti Aapro, President of the European Cancer Organisation, and Ouzna Morsli, EMEAC Oncology Medical Lead at MSD.
Morsli began by saying that progress is being made in addressing the burden of lung cancer. Mortality is falling thanks to reductions in the incidence of the disease and its better management, with greater advances in treatment in the last five years than in the previous twenty.
Nevertheless, a report by the Economist Intelligence Unit showed that there are opportunities for the improvement of care in all countries, with around half of lung cancer guidelines not including fast-tracking of suspected lung cancer patients for diagnostic testing, a specific timeframe for obtaining testing nor rapid referral of newly diagnosed patients for treatment.[15]
There are also delays in lung cancer care all along the pathway. There is therefore a need for the development and implementation of quality indicators, and for the results to be audited.
Insights into Lung Cancer Care
To demonstrate what can be achieved, Hans J.M. Smit, Pulmonologist at Rijnstate Hospital, Arnhem, Netherlands, presented the Dutch Lung Cancer Audit, of which he is Chairman, alongside Rawa Ismail, PharmD and PhD Candidate at the Dutch Institute for Clinical Auditing (DICA).
Smit said the Audit is a multidisciplinary, government-funded register under the umbrella of DICA that began in 2016 and has evolved in the intervening years to cover surgery, radiotherapy and medical therapy. It aims to offer insights into the quality of lung cancer care by focusing on, for example, diagnostics, time to diagnosis and therapy, therapy outcomes, and the provision of best supportive care.
Quality indicators are established by the scientific committee and external parties, such as healthcare insurers and the Dutch Health Care Institute, and are based on national quality standards and evidence- based guidelines. In total, 15 quality indicators were implemented to improve processes and clinical outcomes.
The Audit, which receives data from more than 40,000 lung cancer patients from 73 hospitals throughout Netherlands, has needed to overcome some specific implementation challenges, Smit noted. This has included working to contain the time needed to input data, to ensure control over how the inputted data is processed, and generally to ensure maintenance of privacy standards.
Improving the Quality of Care
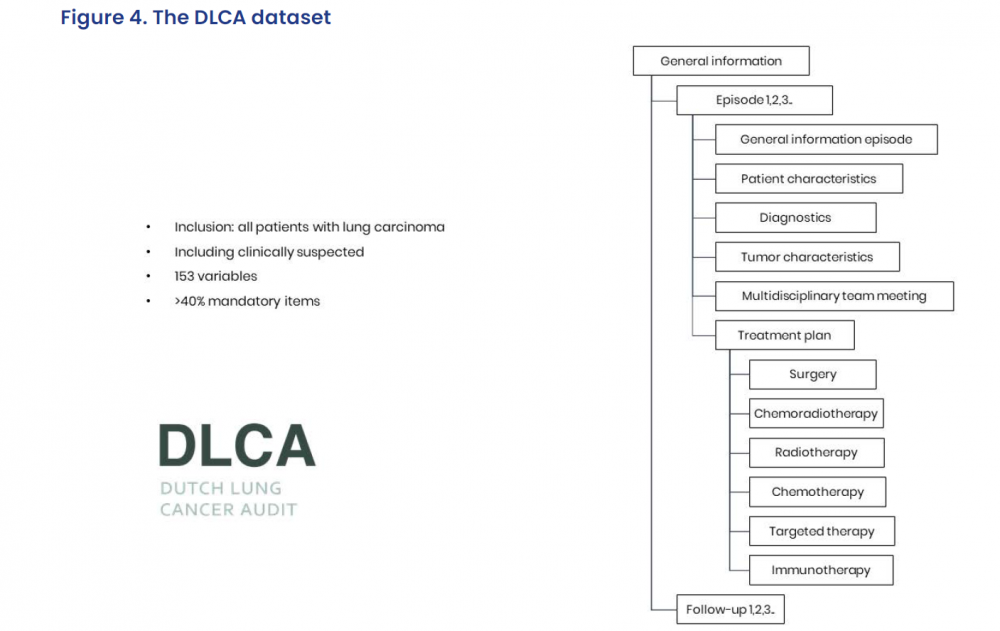
Ismail said that the Audit has nevertheless successfully included all Dutch patients with lung carcinomas, as well as those with suspected disease, gathering data on 153 variables, of which over 40% are mandatory.
The results, the first of which were published in 2020,[16] show that the completeness of the dataset has increased over time, and only two hospitals are seeing fewer than the recommended minimum number of patients.
Crucially, there have been improvements in care over the course of the Audit. For example, the proportion of stage III non-small cell lung cancer patients undergoing brain imaging increased from 82% in 2017 to 90% in 2019, and the proportion of stage IV adenocarcinoma patients receiving molecular diagnostics increased from 89% to 93% over the same period.
The Audit also showed the time from diagnosis to starting treatment was less than 21 days for 62% of patients without invasive mediastinal diagnostics and 46% of those who had endoscopic or endobronchial ultrasound scan, and less than 35 days for 59% of those who had mediastinoscopy.
What this means for clinical practice is that, via standard setting and data analysis, the Audit improves the quality of tumour information and management recommendations, which, combined with patient values and preferences, improves shared decision-making.
Smit said the Audit also shows that, while quality registries play an important role in quality care improvement, and benchmarking with other hospitals can offer best-practice examples, it takes time to initiate a nationwide registry.
It is also important to start small in terms of the number of quality indicators to minimise the burden on hospitals. Nevertheless, indicators on hospital processes can lead to indirect improvements in care and, while outcome measures are of high value, they should be measured only when the registry data are rich and reliable.
An Inspiring Example
In the following discussion, Aapro said that the Audit is a wonderful example of what everyone in lung cancer care could achieve, while Helmut Prosch, from the European Society of Radiology, said benchmarking is important to optimise care pathways and help discussions, and should be rolled out Europe-wide. He underlined that it is only by following best practice that outcomes will improve.
Asked whether patient-reported outcomes are included in the Audit, Smit confirmed that they are, but explained it is not easy to analyse them as survival has historically been very poor in lung cancer. The team are nevertheless looking at ways to integrate them into the registry.
In closing, Morsli said she hopes the Audit will inspire others and, while awaiting Europe’s Beating Cancer Plan, cancer dashboards, including care quality indicators, should be further explored, and collaborations to improve care continued.

