Essential Requirements for Quality Cancer Care: Lung Cancer
Yolande Lievens, Co-Chair of the Essential Requirements for Quality Cancer Care: Lung Cancer, opened the first session by highlighting that the incidence of lung cancer in Europe in 2018 was 365,000 individuals, while mortality reached almost 300,000.
Moreover, prognosis remains poor, with five-year survival rates very low. While the incidence of lung cancer is higher in Western and Northern European countries, the mortality ratio is far higher in Eastern and Southern Europe.
There are opportunities for improvements in the prevention and management of the disease but they remain insufficiently exploited. This will require the better organisation of healthcare to ensure access to multidisciplinary management to drive up both the quality of prevention and care and better outcomes.
The Essential Requirements for Quality Cancer Care (EQRCC): Lung Cancer[1] aim to help countries bridge that gap. Written by experts representing all disciplines involved in cancer care in Europe, the paper gives patients, healthcare professionals and policy makers a guide to essential care throughout the patient journey.
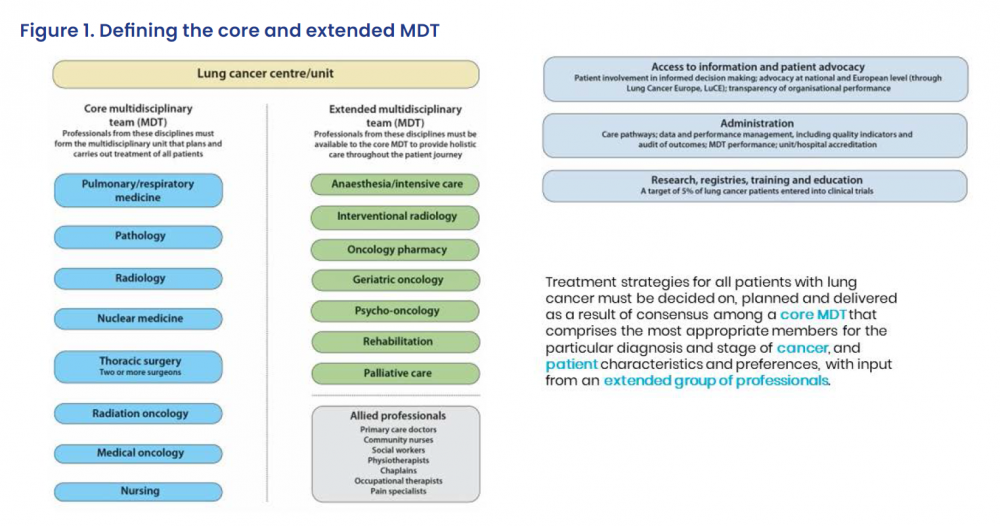
The paper helps cancer centres and healthcare professionals structure and organise care to bring optimal treatment to their patients. The paper gives recommendations on pathways and timelines, on what a cancer centre should look like, the composition and requirements of the core and extended multidisciplinary team (MDT), on patient involvement, performance indicators, and research and education, among others.
They also highlight the challenges around lung cancer. These include the high rate of diagnoses at advanced stages, for which, besides prevention, screening may be a solution alongside improved awareness and education. It sets out strategies to improve primary care and emphasises the complexity of diagnosis and staging.
Optimal treatment is challenging, however, as patients may be older and have comorbidities, and care should be tailored to their needs. The psychosocial needs of people with lung cancer are frequently neglected compared to other cancers, which is partly linked to the stigma surrounding the disease, due to it being often seen as self-inflicted.
Crucially, the quality of care must be measured. Centres must develop performance metrics and quality indicators based on the EQRCC: Lung Cancer and on clinical guidelines, in line with national and legal requirements.
Operational policies are needed to ensure the benefits of a coordinated clinical pathway are realised, alongside effective data management and reporting systems, engagement with patients, their carers and support groups, and accountability over governance processes.
Above all, the EQRCC: Lung Cancer should not remain a static endeavour but be continuously updated to integrate optimised treatment and health system approaches.
Ambitious Engagement
In the following discussion Irena Joveva MEP (Slovenia, Renew Europe) said that 2020 has been marked by ambitious engagement by the European Parliament on cancer policy, with numerous committees and legislative files dedicated to the fight against cancer. However, as access to screening and early diagnosis, as well as cancer survival, is often associated with an individual’s place of birth, there is a need for greater involvement on a European level.
Closing the gaps between countries and regions can be achieved, and Joveva recommended an EU goal be established of doubling survival for poor prognosis tumours such as lung cancer. She hopes that the EU4Health programme[3] will support this aim, and would allow for a Europe-wide cancer dashboard, giving particular attention to lung cancer.
While the impact of the COVID-19 pandemic on screening programmes has made the fight against cancer harder, Joveva believes change is possible, and thanked the European Cancer Organisation for its work in helping to improve cancer care.
Acknowledging the Psychological Impact
Anne-Marie Baird, President of Lung Cancer Europe and Member of the European Cancer Organisation’s Patient Advisory Committee, said the EQRCC: Lung Cancer could have a huge impact all along the care pathway, and agreed that it must continue to evolve.
Cooperation will be key to implementing screening, as although there have been policy changes across Europe, they have not been widely implemented. Early detection, on the other hand, relies heavily on education and awareness for both the public and medical professionals. It is not acceptable that any part of the care pathway delays diagnosis or treatment, as people impacted do not have the luxury of time. Access to best care cannot wait.
Baird also stressed the huge psychological impact of lung cancer, and the issues around access to support, as well as the financial toxicity associated with cancer.
She welcomed the emphasis in the Essential Requirements on securing access for the patient to the multidisciplinary team (MDT) but stressed this was too often not the reality experienced by patients. Metrics should be used to demonstrate improvements in care, and allow patient groups to lobby for better care. Information is ammunition for driving and influencing policy changes, as well as driving the optimisation of the care pathway.
Lievens said she fully agreed with the points raised by Baird, and said she is looking forward to collaborating to turn them into action.

