Improving Outcomes with Data-Driven Care: Tackling the East–West Divide
The East-West Divide session was chaired Matti Aapro, President of the European Cancer Organisation & EU Cancer Mission Assembly Member and co-chaired with Linda Gibbs, Oncology Lead for Central/Eastern Europe, Pfizer.
Pan-European Cooperation
At the start of the session, John Ryan, Director for Public Health, DG SANTE, European Commission, said that the EU is aware of the health inequalities that exist across Europe, which are revealed in the dramatic differences in life expectancy not only between but also within member states.
He emphasised the importance of ensuring that the introduction of improvements in cancer care does not increase the gap between the countries but rather bring those at the bottom closer to those at the top. This will require the mobilisation of support at the EU level, where equal access to care is a key issue.
With Europe’s Beating Cancer Plan, he said, there is an opportunity to include specific provisions to tackle inequalities, not just in terms of grants and funding but also policies for legislative changes to improve cancer screening and uptake, encourage best practice and improve access to innovation.
Maria Carvalho, MEP, Portugal, agreed that tackling the East-West divide is about narrowing the gap between regions and countries. More than that, it is related to issues of cooperation and coordination between various stakeholders and between countries.
While there is a drive to increase cancer care budgets, the proposed Horizon Europe programme should focus not only on money but also on cooperation across all areas of care, including twinning between countries in different regions of Europe.
This, she said, should be underpinned by more clinical research, which has been shown to be clearly linked to improvements in healthcare outcomes.
Benchmarking Optimal Care with the Cancer Dashboard
Professor Mark Lawler, European Cancer Organisation Board Member, and Associate Pro-Vice Chancellor and Professor of Digital Health, Queen’s University Belfast, said that, despite the current challenges due to the COVID-19 pandemic, there have been chinks of light in recent years. Health has been established as an EU priority, and cancer has become a clear area of focus through Europe’s Beating Cancer Plan and the EU Cancer Mission.
Lawler emphasised that it is absolutely critical that the opportunities offered by the political momentum around cancer in Europe are grasped, but equally important that these opportunities be used wisely. He also underlined that the European Code of Cancer Practice and its implementation offers an unrivalled opportunity to address the cancer inequalities that many European face every day.
The diverging incidence and mortality rates for cancer across Europe are multifactorial in nature. Healthcare expenditure is a challenge, and it is notable that total healthcare spending across Central and Eastern European (CEE) countries is below the EU average. While some countries in the region are outspending their peers, this is not reflected in improved outcomes, highlighting that it is not necessarily what you spend but how you spend it.
Lawler stressed the absolute primacy of appropriately resourced, data-enabled NCCPs. Data and cancer intelligence must be deployed to ensure that local and regional contexts are captured, and that funding is appropriately allocated. Data can also highlight health inequalities, and empower clinical research to be focused in the right areas. Nevertheless, some CEE countries still do not have an implemented, appropriately resourced NCCP.
The Central and Eastern European Cancer Action Group, which involves a range of stakeholders from the region, was established over three years ago to review the cancer landscape in CEE countries, collect cancer intelligence and develop tools to help improve care. Four recommendations were made: invest in research education and training; standardise patient pathways, enhance capacity; and patient advocacy.
Crucial to this aspiration is the development of a cancer learning environment that highlights key challenges and inequalities, and allows progress to be measured and best practice to be benchmarked. To achieve this, a CTRL Cancer Country Dashboard was developed, offering an easy-to-use tool for visualising the current status of cancer care and research. The tool, which covers 16 CEE countries, also allows monitoring and benchmarking of progress on key components within each NCCP.
Meeting the challenges of implementing a cancer plan
Véronique Trillet-Lenoir MEP, Lead Rapporteur for the Special Committee on Europe’s Beating Cancer Plan, introduced the next section of the session, which focused on three recently developed NCCPs from CEE countries: Slovenia, Poland and Croatia.
She emphasised that there is much to learn from the experience of others, and successful initiatives must be built upon in a collaborative way so that in-country knowledge and best-practice can be exchanged.
Mapping services and international collaboration
Professor Tit Albreht, Head of the Centre for Health Care, National Institute of Public Health, Slovenia, said that their cancer registry, one of the oldest in the world, has allowed for the very precise monitoring of cancer data and, through the introduction of screening programmes, they have been able to significantly lower cancer incidence and mortality.
Slovenia has also produced two NCCPs, the first tailored to mapping cancer services and ensuring access to high quality care, the second focused on survivorship. Within these NCCPs, they have improved multidisciplinary care, allocated funds, concentrated on infrequent cancers and developed a joint guideline with GPs on pain management, despite many challenges along the way.
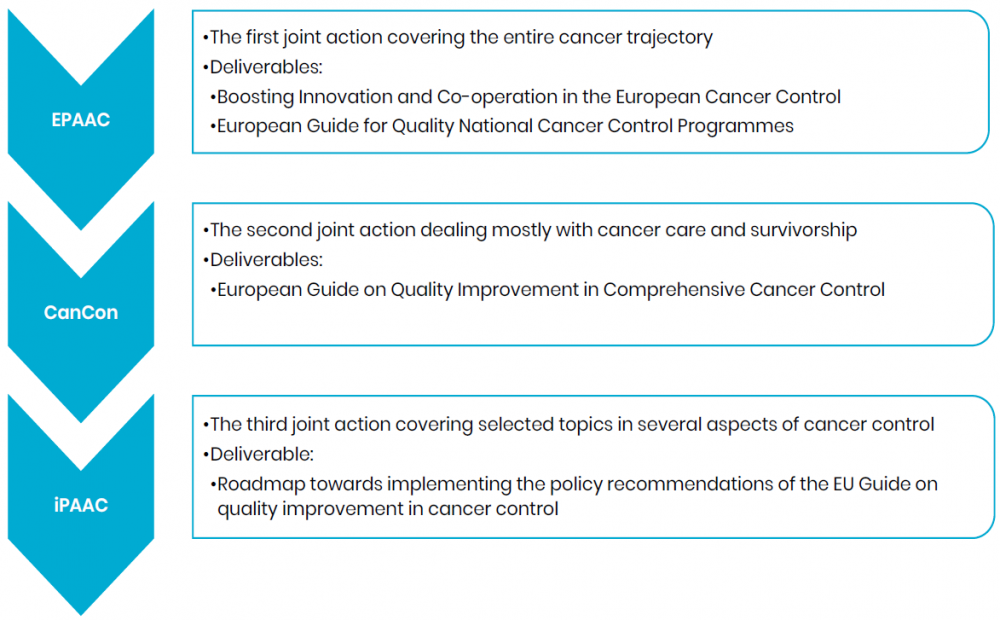
The country has a clear commitment to cancer care and has been closely involved in cancer policy at a European level, through initiatives such as the European Partnership for Action Against Cancer. This led to the development of a roadmap for implementing the recommendations of the European Guide on Quality Improvement in Comprehensive Cancer Control, and involvement in the Innovative Partnership for Action Against Cancer (Figure 3).
Figure 3. Slovenia’s Involvement in the European Cancer Policy
Tackling inequalities at all levels of care
Professor Piotr Rutkowski, Professor, Surgical Oncology, Maria Sklodowska-Curie National Research Institute of Oncology, said that it is estimated that 50% of cancer deaths in Poland are preventable, and the incidence of the disease is set to rise by 28% in the next decade.
In response, the Polish NCCP was launched in February 2020, with a focus on health education and promotion, early detection, diagnosis and treatment, access to high-quality care and clinical research.
Setting targets for breast, cervical, colorectal and lung cancer, as well as melanoma, they developed five areas that needed to be resourced: medical staff, education and prevention, secondary prevention, science and innovation, and a cancer care system (Figure 4).
Figure 4. National Cancer Plan – Scheme
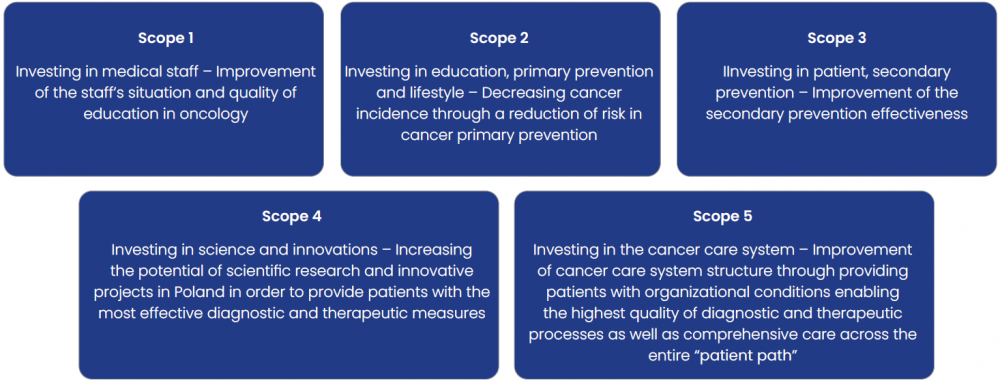
Within those areas, there are a range of actions and measures to improve the coordination of cancer care, the development of standards and guidelines, support for patients during and after therapy, the establishment of cancer units and a new national oncology portal, and the digitalisation of the national cancer registry.
Data-driven targets and clear frameworks
Professor Eduard Vrdoljak, Head, Center for Oncology and Professor, Faculty of Medicine, University of Split, said that Croatia was in desperate need for an NCCP, as the mortality rate among male cancer patients, for example, was twice as high as that in Denmark.
A group of stakeholders assessed the magnitude of the problem, set measurable objectives, evaluated evidence-based strategies for cancer control and prevention, and identified their priorities for initial activities.
Working with foreign experts, they developed, over three years, an NCCP that covered the entire spectrum of cancer care, from prevention topalliation and beyond, into education and research, based around three initial priorities (Figure 5).
Figure 5. Choosing Priorities for Initial Cancer Control Activities
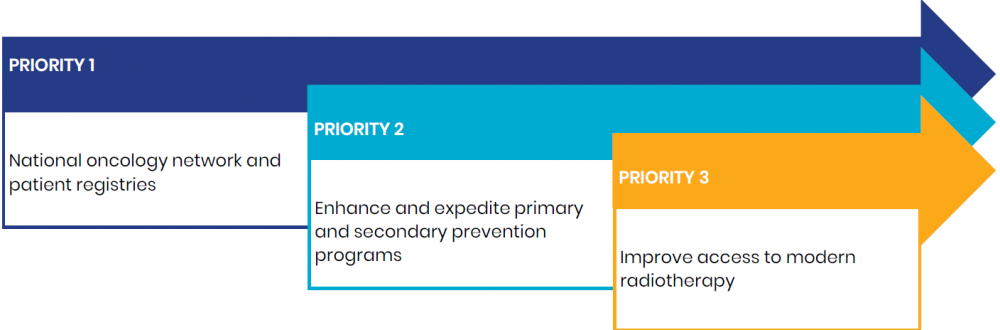
The NCCP set data-driven targets around smoking, alcohol consumption and obesity measures for primary prevention, early detection for key cancers, and a framework for increased participation in cancer research that incorporated legislation, infrastructure and promotion to healthcare professionals and the public.
This can lead to huge gains in quality-adjusted life years at an average cost far below the World Health Organization recommended GDP per capita threshold for cost-effective care.
Ensuring Cancer Plans Become Reality
The East-West Divide session was co-chaired by Linda Gibbs, Oncology Lead for Central/Eastern Europe, Pfizer.
“Despite encouraging advances in science and technology, the inequality gap between CEE and Western European countries continues to rise. This is highlighted by mortality rates for disease such as lung and cervical cancer, as well as breast and rectal cancer, being distinctly higher in CEE countries.”
“Making effective change a reality in cancer control across Europe will require collaboration between stakeholders, including policy experts, patient groups, government and industry, alongside robust cancer data. The momentum created by Europe’s Beating Cancer Plan and the experiences of countries such as Slovenia, Poland and Croatia must also be harnessed. Working together, we can drive change in cancer control, improve patient outcomes and close the inequality gap.”

