Introduction
By Matti Aapro, President of the European Cancer Organisation & EU Cancer Mission Assembly Member
Inequalities are sadly a feature of cancer care, not just in Europe but all around the world. They reflect all aspects of life, in which a patient’s age, sex, gender, level of education, socioeconomic status, disabilities and, crucially, location can have a major impact on the quality of cancer care they receive.
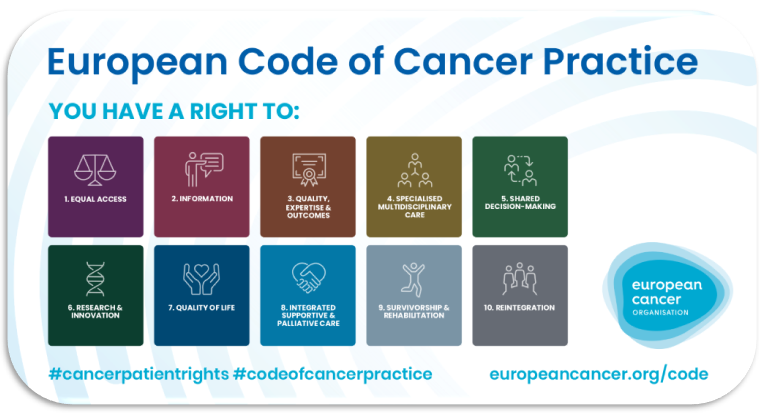
The European Code of Cancer Practice enshrines a series of ten overarching rights for patients, and in particular signposts what patients should expect from their health system, in order for them to achieve the best possible outcomes.
However, it is a reality of cancer care in Europe today that many patients cannot enjoy those rights, and it is only through coordinated action and policy developments at local, national and regional levels that the aim of equal access to high-quality cancer care for all will be realised.
Bringing the Community Together to Tackle Inequalities
The Community 365 Roundtable on Inequalities was our first Community 365 Roundtable, since this initiative was launched in January 2020. These meetings bring together charity, philanthropy and industry contributors to the Focused Topic Networks of the European Cancer Organisation, with the aim of providing ideas, guidance, practical support and resources for building consensus in the European cancer community.
The topic of Inequalities was chosen for the first Roundtable not least because of the importance placed on the subject by the EU Health Commissioner, Stella Kyriakides, in previous meetings with our Member Societies and Patient Advisory Committee, as well as in the forthcoming Europe’s Beating Cancer Plan.
The Inequalities Network, led by Co-Chairs Dr Nicolò Matteo Luca Battisti, SIOG President-Elect, and Professor Hendrik Van Poppel, EAU Adjunct Secretary General, aims to shine a spotlight on the cancer inequalities, so that readily available policy mechanisms can be enacted to bridge gaps and raise standards and outcomes in cancer care across all of Europe, for all groups in society. In so doing, the Network builds on the existing work of Network participants, and liaises closely with the EU institutions and others in providing advice and recommendations.
With collaboration on the programme of Sanofi and Pfizer representatives, this Roundtable, held on 14 October 2020, brought together policy-makers, politicians, oncology experts and patient advocates to discuss important areas of inequality in cancer care in the weeks before the launch of Europe’s Beating Cancer Plan in December in two dedicated, in-depth sessions:
• Treating Ageing Patients with Cancer
• The East-West Divide
These highlighted the wide-ranging issues faced by the ageing patient with cancer and those in less advantaged areas of Europe.
Underpinning both topics is the absolute need for the development, in collaboration with regional experts, of a comprehensive, data-driven and fully implemented national cancer control plan (NCCP). These must build on a thorough understanding of the local cancer care landscape to tackle inequalities all along the cancer pathway, from screening and prevention through diagnosis and treatment to survivorship and palliative care, underpinned by clinical research and innovation.
Treating the Ageing Patient with Dignity
For the ageing cancer patient, addressing inequalities in cancer care means first and foremost that they must no longer be treated based on their age but rather on who they are as a person. This must take into account their health status, associated comorbidities and socioeconomic situation. In other words, they must be treated with dignity.
This must stretch beyond their immediate cancer care and be reflected in the way research is conducted for cancer therapies. Older patients have been systemically excluded from clinical trials, where the focus has been on younger patients with a good performance status. The result is that there is a dearth of evidence on the efficacy and safety of medications in older individuals with multiple comorbidities, as well as on optimum radiotherapy schedules or even the expected outcomes of surgical interventions.
To better tailor management, oncologists must work closely with geriatricians to develop age-appropriate care plans. In line with Right 4 of the European Code of Cancer Practice, multidisciplinary and multi-professional care is fundamental to the provision of best quality cancer care to any cancer patient. For older patients, potentially with multiple conditions, this includes such elements as pharmacist assistance in the management of polypharmacy. The concept of multi-professional care must also be expanded to include general practitioners, so that care is no longer denied to patients simply based on their age and that they receive appropriate follow-up once outside the hospital.
The example of France has shown how the specific inclusion of older patients in the NCCP can lead to the identification of key priorities and the establishment of networks of geriatric oncology centres, as well as national guidelines and specialist training.
National Cancer Control Plans Reflecting Local Contexts
The East-West divide has come under the spotlight recently, with key figures at the European Union (EU) recognising the need to address the often stark inequalities that exist between and within countries, which are associated with large disparities in cancer survival.
Increased funding for healthcare, while an important factor in ensuring equitable care, is not the only answer, however. Access to reliable data and robust evaluation are both critical factors in identifying priorities and developing cancer policies that reflect the local context.
In recent years, countries such as Slovenia have made huge strides in improving cancer care through the development of a modern NCCP in collaboration with experts from across the region. These plans must focus not only on access to innovation but also on comprehensive cancer reporting through population-based cancer registries, health education and health promotion, improvements in cancer screening, early detection and treatment, and survivorship issues.
Another crucial aspect is participation in clinical trials and research, as it has been shown time and again that clinical research is a key determinant of improvements in cancer care, all of which underscores the need for stakeholder collaboration across sectors and borders in the region.
We have seen that, through determined effort and coordinated policy initiatives, inequalities can be reduced and progress can be made. The opportunity is there and it is up to us to seize it. We must work together to drive change: The time for action is NOW.
Action Points for Tackling Inequalities in Cancer Care
The Ageing Patient
• Treatment should no longer be chosen based on a patient’s chronological age but on a comprehensive understanding of their health status and circumstances
• Surgical, radiation and medical oncologists must routinely use geriatric assessment tools and work in conjunction with geriatricians to develop joint care plans
• Older patients must be included in clinical trials to broaden the evidence base and allow treatment optimisation
• General practitioners and other healthcare professionals must be included in ongoing follow-up to ensure better understanding of the individual’s circumstances and better access to personalised care
• Older patients must be specifically named in national cancer plans to develop national guidelines and establish specialised treatment centres
The East-West Divide
• An evidence-based approach to decision-making and policy development via a national cancer control plan is essential to achieving affordable, equitable cancer control
• Cancer control must be driven by robust cancer monitoring and reporting and comprehensive cancer intelligence to allow a detailed understanding of the local cancer landscape
• Multidisciplinary care and standardised treatment pathways must be developed to ensure quality care along the patient pathway and the optimal use of resources
• A learning environment must be developed to highlight key challenges and inequalities and measure progress and benchmark best practice.