Early Detection and Screening
The session was co-chaired by Matti Aapro, President of the European Cancer Organisation, and Françoise Bartoli, Vice-President, Head of Europe and Canada, Oncology Business, AstraZeneca. Bartoli began by underling that everyone taking part in the Roundtable meeting shared a common vision to build a better future for lung cancer patients.
She noted that the EU Mission Board for Cancer set a target of saving three million lives by 2030. [4] However, lung cancer accounts for one in five deaths worldwide, and any reduction in mortality will have a significant impact on overall cancer deaths. The past few years have seen considerable advances in treatment options for lung cancer, yet the prognosis remains very low.
While there are clearly challenges, there are also opportunities, and progress will transform lives. Targeted screening and early detection programmes have been piloted in some countries, such as France, Germany and the UK, and there is a move towards national implementation across Europe. However, the COVID-19 pandemic has intensified the need to act urgently, as any delays will have an enormous impact further down the line.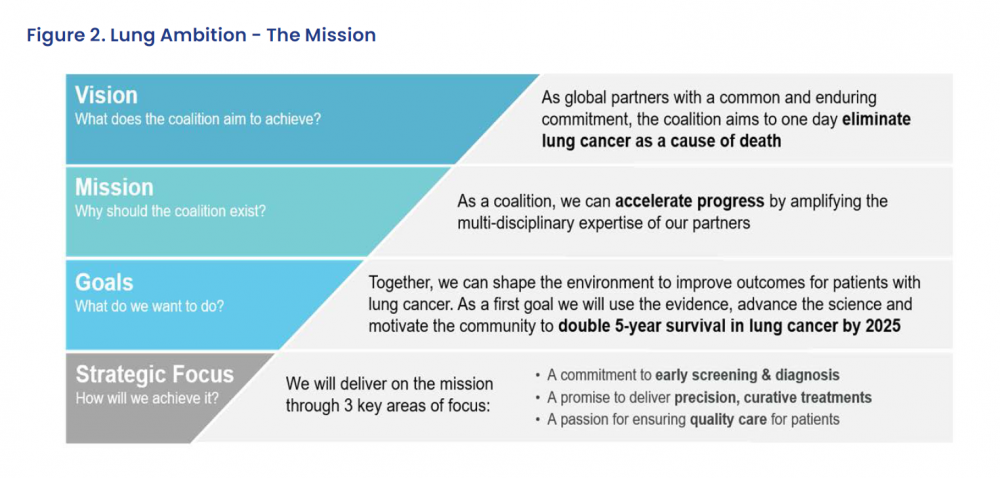
Collaboration Key to Tackling Lung Cancer
Giorgio Scagliotti, Professor of Medical Oncology, University of Turin and Chief of the Medical Oncology Division at the S. Luigi Hospital, is Past President of the International Association for the Study of Lung Cancer (IASLC). He explained that accelerating advances in lung cancer care requires collaboration, and that is at the heart of the current strategic plan of the IASLC.
Lung cancer remains a huge challenge, however, with almost two million people dying from the disease worldwide every year. While five-year survival of patients with stage I/II disease is around 60%, only just over a quarter are diagnosed in early stages. In contrast, 40% of patients are diagnosed in stage IV, when five-year survival is 10% or less.[5,6]
Scagliotti explained that the IASLC is currently gathering data for the ninth edition of the TNM Classification for lung cancer, due in 2024. This will include, for the first time, information on gene alterations and protein expression, at least in a subgroup of patients included in the database, with the aim of achieving more precise diagnosis and treatment and, ultimately, improved patient survival.
In addition, the Lung Ambition Alliance has been launched,[7] for which the IASLC has joined forces with industry partners and no-profit organisations to accelerate progress towards eliminating lung cancer as a cause of death, with the initial goal being to double five-year survival by 2025. This will be underpinned by a focus on early screening and diagnosis and the delivery of precision, curative treatments, as part of quality healthcare.
Scagliotti emphasised that results from screening trials have shown that, despite the different methods and models used across the various studies, mortality is reduced by 20%–40%. However, key issues remain, despite the evidence from randomised controlled trials, the optimal screening frequency, the potential for over-treatment and over-surveillance, the long-term outcomes, as well as unresolved questions about the role of biomarkers.
One of the major barrier to screening uptake remains the lack of awareness and understanding of its benefits and effectiveness, particularly among primary care physicians. There are also ongoing considerations around the planning and implementation of screening, such as the identification of high-risk, hard-to-reach populations, public recruitment to and engagement with screening, , differences in lung cancer incidence between men and women, and the cost-effectiveness of combined screening and smoking cessation.
Some of these issues are being explored by the Early Lung Imaging Confederation (ELIC),[8] which aims to integrate deep learning and artificial intelligence approaches towards the early detection of lung cancer. This includes image analysis and stratification and it will represent a research tool to identify patients requiring non-invasive biomarker studies or invasive procedures. There are also a number of promising lung cancer screening biomarkers under investigation, including nucleic acids, cells, proteins and other molecules detectable in the blood, bronchoscopy samples, sputum and exhaled breath, among other sources.
Another initiative, the Major Pathologic Response project, will combine recommendations on standardised tissue processing and pathologic assessment with big data to use major pathologic response as a surrogate marker for survival.
These and other projects, such as ILC2,[9] and TERAVOLT,[10] aim to leverage enhanced data sharing and analysis to identify tumour characteristics that be used to ultimately improve the survival of lung cancer patients.
A Window of Opportunity
In the following discussion, Frances Fitzgerald MEP (Ireland, EPP) said the COVID-19 pandemic has been very challenging in terms of cancer care but has led to a debate over EU legal competencies to act in areas of health policy, which may offer future opportunities to improve pan-European collaboration on topics such as lung cancer. Indeed, there is a new emphasis and desire to work together on health in general and on cancer in particular, as illustrated by the forthcoming Europe’s Beating Cancer Plan,[11] and the numerous committees
working actively in this area.
She believes that there is a window of opportunity, and a great deal of motivation, to build bridges and share research, information and best practices to develop the best policies to tackle the challenges faced in cancer care. Key to this are multi-stakeholder groups and partnerships, alongside awareness campaigns to translate specialist knowledge and research for the public.
Breast cancer is a great example of this but lung cancer is currently lagging behind. More work is therefore needed in this area. Cancers are generally considered blame-free but lung cancer is often seen as self-inflicted, and patients may blame themselves for their illness. This has to be tackled while making sure that young people understand the risks of smoking.
Fitzgerald hopes that Europe’s Beating Cancer Plan will help to bring the best of European research to patients, especially as many EU Member States are slow to implement innovations. The aim must be to use the lessons of the COVID-19 pandemic to bring people and organisations together to drive improvements in lung cancer care.
Preparing the Ground for Screening
Helmut Prosch, from the European Society of Radiology, agreed with those sentiments, saying that if the international and local efforts in the fight against COVID-19 were repeated for lung cancer, there could be huge strides in diagnosis, treatment and care.
He underlined that lung cancer screening requires collaboration not just between patients and clinicians but also with politicians, especially in tackling the stigma surrounding the disease. The supportive evidence is already there, but implementation studies are required to convince clinicians and policymakers of its worth.
Jan van Meerbeeck, from the European Respiratory Society, echoed those comments, saying that, although screening should be considered the standard of care in lung care, the issue remains its implementation.
Scagliotti observed that lung cancer screening should be used as a preventive measure in those considered at high risk but said he would not advocate starting screening in community hospitals right away, as the right framework is required and the ground needs to be prepared. However, he emphasised that the pandemic has shown what was considered impossible just one year ago is seen as possible today, and so the initiative should be seized to take these efforts forward.
Implications Further Along the Treatment Pathway
Marc Beishon, co-author of the Essential Requirements for Quality Cancer Care: Lung Cancer, commented that screening could raise issues further along the treatment pathway as, if it becomes widespread public policy, it will have implications for lung cancer centres by increasing patient numbers.
Yolande Lievens, Co-Chair of the Essential Requirements for Quality Cancer Care: Lung Cancer, agreed, saying that how to address the availability of resources needed for treatment will have to be considered. She also underlined Fitzgerald’s comments on awareness over the risks of smoking, not least in younger people, as it remains of the utmost importance as a key pillar in the fight against lung cancer. Moreover, it is supported by all professionals in the field.
In closing, Bartoli said the session showed that, despite the variety of perspectives, there is clearly a very strong commitment to the early detection and screening of lung cancer.