The Cancer Control Context
The focus of The Code is on the care experienced by patients and the outcomes achieved, through the high quality diagnosis, treatment and care that they need throughout their cancer journey. However, the planning of cancer care at every level must be sensitive to the patterns of cancer incidence and the mortality from cancer in each country and population. The pattern of cancer incidence in a country determines the number of cancer patients overall, the nature of their cancer diagnoses, and the burden experienced by each patient and the health service.
In their recent Comparator Report on Cancer in Europe 2019 (6), the Swedish Institute for Health Economics has comprehensively described the context for good cancer control. The incidence of cancer is determined by the growth in the population, the ageing of the population (because cancer incidence is strongly age-related), and by the prevalence of risk factors including smoking, obesity, alcohol consumption, ultraviolet radiation in sunshine, occupational exposures etc (6). The estimated number of cancers in Europe in 1995 was 2.055 million people; in 2018 it had increased to 3.081 million people (6). The European population is ageing and the proportion of people aged 60 years and older has increased from 20% to 26% (6). The impact of the ageing population can be standardised statistically to produce Age Standardised Incidence Rates, which allow evaluation of the underlying trends in cancer incidence due to factors other than aging. When this is done, there is still evidence of increasing cancer incidence between 1995 and 2018 shown in Figures 1 and 2 in most countries and a substantial variation between European countries, most of which need to improve their planning for cancer prevention, early diagnosis, treatment and care.
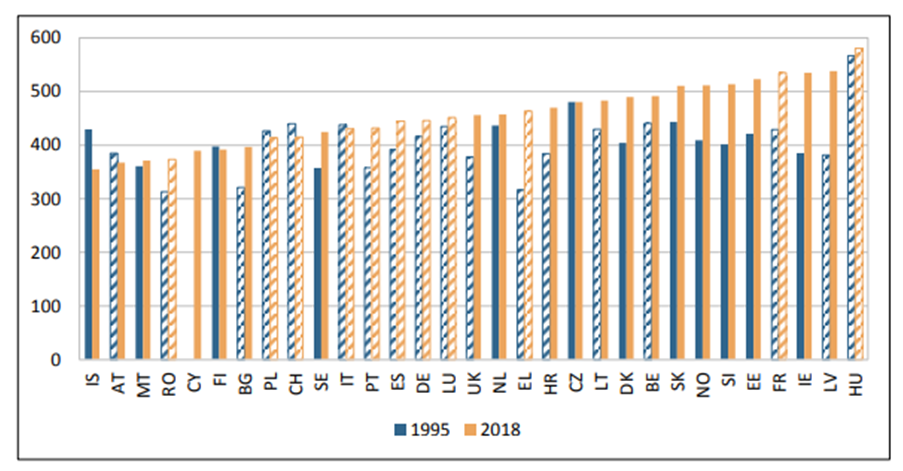 Figure 1. Cancer incidence in men per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018 in 31 European countries (6). Hatched bars are based on regional data or neighbouring countries in all Figures
Figure 1. Cancer incidence in men per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018 in 31 European countries (6). Hatched bars are based on regional data or neighbouring countries in all Figures
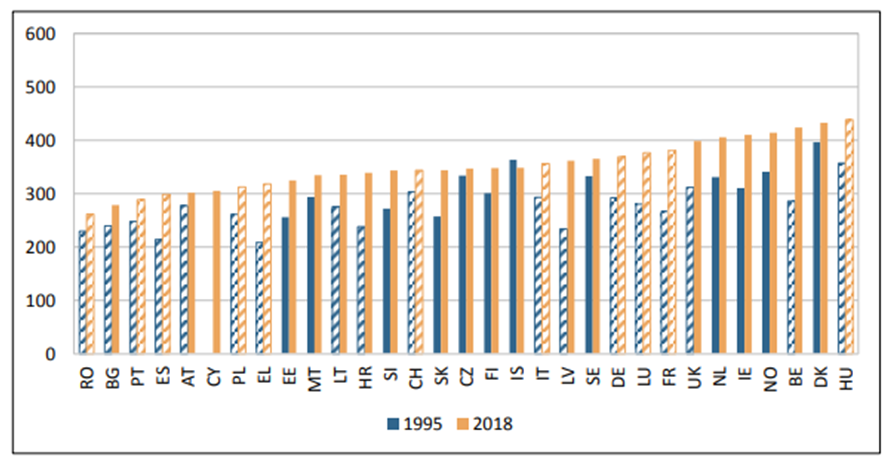
Figure 2. Cancer incidence in women per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018(6). Hatched bars are based on regional data or neighbouring countries in all Figures
In men (Figure 1), the incidence rates for cancer have increased in the majority of countries; however, Iceland, Austria, Finland, Poland, Switzerland, Italy and Czechia have recorded slight decreases. In women (Figure 2), incidence rates have increased in all countries except Iceland. Factors which have influenced this variation include the increase in obesity and alcohol consumption and the reduction of smoking in many countries.
The complex series of factors which influence cancer incidence have different effects on different cancer types. For example, the decline in smoking would be expected to influence lung cancer more than most other cancer types. The shifting pattern of the most common cancers diagnosed in European men between 1995 and 2018 is shown in Figure 3.
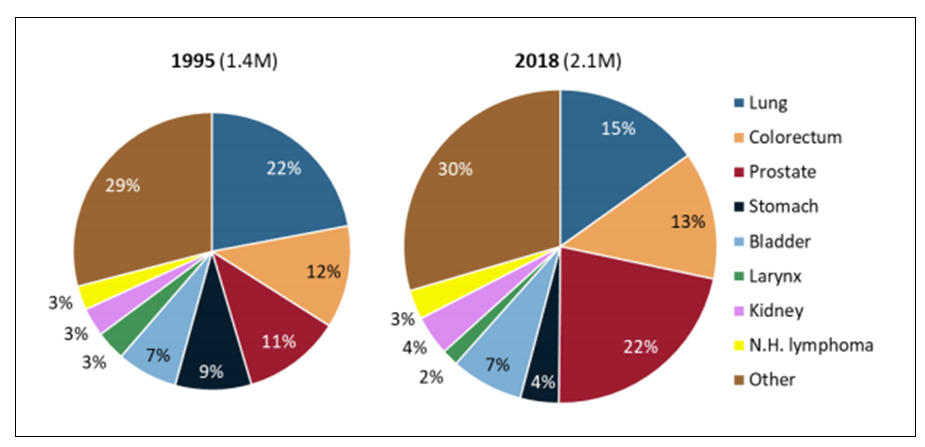
Figure 3. Most common cancer types diagnosed in men in 1995 and their share in 2018, Europe (6)
Cancer mortality, the total of number of deaths from cancer, has also increased, from 1.191 million in 1995 to 1.445 million in 2018, reflecting the increasing number of cancer cases and the aging population (6, 32). The increasing age of Europeans results not only in a higher incidence of cancer which in itself leads to more cancer deaths, but also there is good evidence that older cancer patients have poorer survival overall than younger cancer patients, which will also increase the total mortality from cancer (32-35). However, there are important and positive features to the changes in cancer mortality. The cancer mortality in European countries can be age-standardised to allow for changes observed that are due to a country’s ageing population. Age standardised cancer mortality has fallen in men and in women in most European countries (Figures 4 and 5) (6).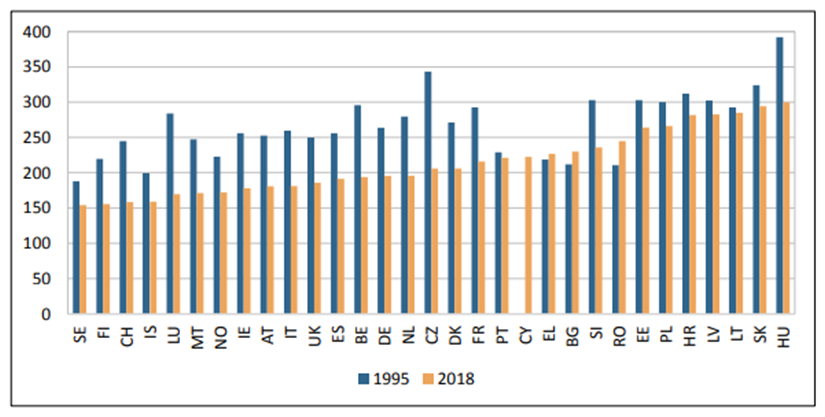
Figure 4. Cancer mortality in European men per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018 (6). Hatched bars are based on regional data or neighbouring countries in all Figures
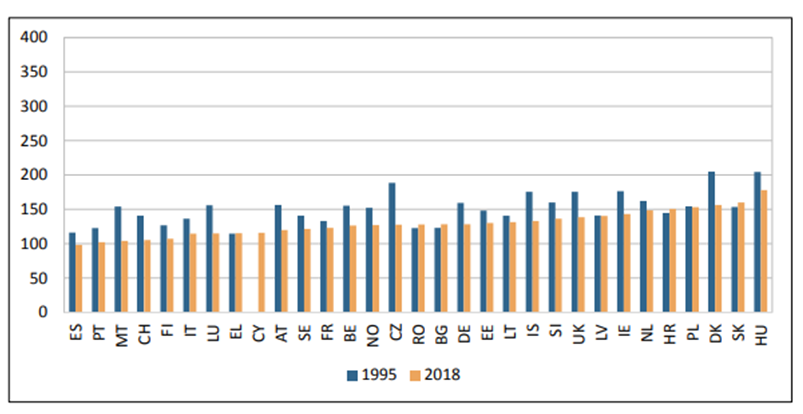 Figure 5. Cancer mortality in European women per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018 (6). Hatched bars are based on regional data or neighbouring countries in all Figures
Figure 5. Cancer mortality in European women per 100,000 inhabitants (age-standardized rates (Old European standard)), 1995–2018 (6). Hatched bars are based on regional data or neighbouring countries in all Figures
However, it is important to note that cancer mortality is changing in different directions in different age groups (Figure 6).
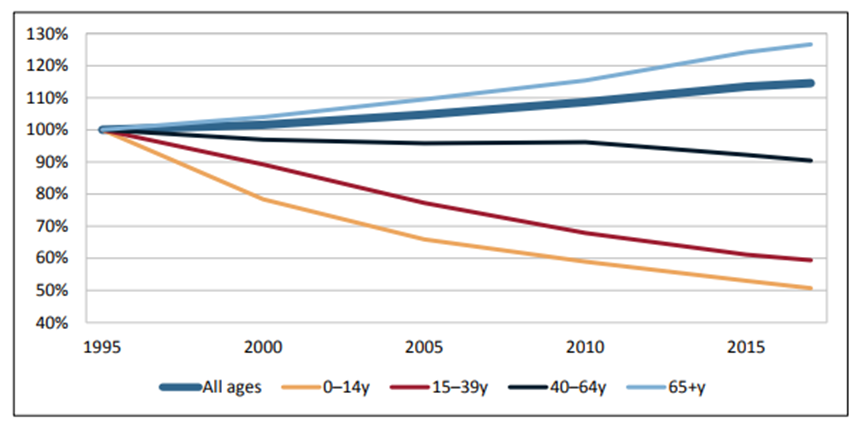 Figure 6. Cancer mortality by age group in Europe (1995=base year), 1995 –2017 (6)
Figure 6. Cancer mortality by age group in Europe (1995=base year), 1995 –2017 (6)
Younger people diagnosed with cancer, up to the age of 64 years, are showing improvements in cancer mortality. The influence of age on outcome has been emphasised by many investigators and is likely to be a complex interaction of patient fitness to undergo diagnostic and treatment procedures, patient and professional attitudes to the diagnosis and treatment of cancer in older people and healthcare access issues for older people (32-35)
These observations set the context for planning to deliver the best available cancer care. The changing patterns of disease types is exemplified by the falling proportion of lung cancer cases, which has positive implications for the burden of that disease on patients and healthcare systems. On the other hand, the age of cancer patients and the number of older people with cancer is growing and represent a powerful challenge to healthcare for cancer patients and to the planning of the delivery of good clinical cancer practice.
Back to Medical Literature and Evidence for the European Code of Cancer Practice


